Wayne State University is embarking on a bold and transformative journey with its Strategic Direction Network 2025 (SDN 2025). This ambitious initiative aims to propel the university to unprecedented heights, empowering it to become a preeminent urban research institution renowned for its impact on the community, the nation, and the world. With a clear vision and a steadfast commitment to excellence, Wayne State is poised to redefine the boundaries of higher education and establish itself as a beacon of innovation and progress.
At the heart of SDN 2025 lies a profound understanding of the university’s unique strengths and the challenges facing our rapidly evolving society. Wayne State recognizes the critical role it plays in preparing students to navigate the complexities of the 21st century. Through a dynamic and interdisciplinary approach, the university is fostering an environment where students can develop the skills, knowledge, and critical thinking abilities necessary to succeed in their chosen fields and make meaningful contributions to their communities.
Furthermore, SDN 2025 emphasizes the importance of research and scholarship as catalysts for progress. Wayne State is investing heavily in its research infrastructure and fostering collaborations with industry and community partners. This commitment to discovery and innovation will enable the university to address pressing global issues, from climate change to social inequality, and generate transformative solutions that benefit humanity. By embracing an entrepreneurial spirit and fostering a culture of creativity, Wayne State is positioning itself as a hub for groundbreaking research and a driving force behind economic development.
Embracing Innovation in Healthcare Education: Wayne State University’s School of Nursing in 2025
Leveraging Technology for Enhanced Learning and Simulation
Wayne State University’s School of Nursing (WSUSON) is at the forefront of harnessing technology to revolutionize healthcare education. In 2025, the school will continue to embrace cutting-edge innovations, creating a transformative learning environment for its students.
One key focus is the integration of virtual reality (VR) and augmented reality (AR) into the curriculum. These technologies will provide immersive simulations, allowing students to engage in realistic clinical experiences from the safety of a classroom. By simulating complex scenarios and medical procedures, students can refine their skills without the need for live patients, ensuring a safe and efficient training environment.
Additionally, WSUSON will implement artificial intelligence (AI) to enhance personalized learning. AI-powered platforms will analyze student performance and provide tailored feedback, identifying areas for improvement and suggesting individualized learning paths. This adaptive approach will empower students to progress at their own pace, maximizing their learning outcomes.
| Technology |
Application |
| Virtual Reality (VR) |
Immersive clinical simulations |
| Augmented Reality (AR) |
Superimposed medical data and visualizations |
| Artificial Intelligence (AI) |
Personalized performance analysis and feedback |
Redefining Nursing Practice through Technology and Collaboration
Leveraging Technology to Enhance Patient Care
Wayne State University School of Nursing (SDN) is embracing technology to transform the delivery of nursing care. The school has invested in cutting-edge simulation labs, electronic health records, and virtual reality tools. These technologies provide students with hands-on practice in realistic clinical scenarios, enabling them to develop essential skills and enhance their preparedness for real-world settings.
Bridging Gaps through Interdisciplinary Collaboration
Recognizing the importance of interdisciplinary collaboration in patient care, SDN has established partnerships with other health sciences schools within Wayne State University and beyond. Through these collaborations, nursing students work alongside medical, pharmacy, and other healthcare professionals to gain a comprehensive understanding of patient needs and develop integrated care plans. This interdisciplinary approach fosters a team-based mindset and prepares students to effectively navigate the complex healthcare system.
Benefits of Interdisciplinary Collaboration
| Benefit |
| Enhanced patient outcomes through coordinated care |
| Improved communication and coordination among healthcare providers |
| Reduced medical errors and increased patient safety |
| Development of innovative and patient-centered solutions |
| Foster a culture of respect and trust among healthcare professionals |
Fostering Interdisciplinary Excellence: Partnerships for Enhanced Patient Outcomes
Team-Based Approach to Patient Care
Interdisciplinary teams, comprising health professionals from various disciplines, provide a comprehensive approach to patient care. This model fosters collaboration and shared decision-making, ensuring that patients benefit from the expertise of each team member. By working together, healthcare professionals can address the complex needs of patients and optimize treatment outcomes.
Collaborative Research and Innovation
Partnerships between academia, healthcare institutions, and industry facilitate innovative research initiatives. Interdisciplinary research teams bring together diverse perspectives and expertise, leading to advancements in diagnosis, treatment, and rehabilitation. This collaboration enhances the translation of research findings into clinical practice, ultimately improving patient outcomes.
Integrated Education and Training
Interdisciplinary education and training programs foster a collaborative mindset among future health professionals. Students from different disciplines learn to work together effectively, developing communication, teamwork, and problem-solving skills. These programs provide a foundation for interdisciplinary patient care and prepare graduates to navigate the complexities of modern healthcare delivery systems.
| Discipline 1 |
Discipline 2 |
Discipline 3 |
| Medicine |
Nursing |
Pharmacy |
| Rehabilitation |
Social Work |
Psychology |
Advancing Health Equity Through Culturally Competent Nursing Care
Providing culturally competent nursing care is paramount to advancing health equity. It ensures that all patients receive care tailored to their unique cultural values, beliefs, and preferences. Culturally competent nurses are equipped with the knowledge, skills, and attitudes necessary to deliver patient-centered care that respects and values diversity.
4. Improving Health Outcomes Through Cultural Understanding
Cultural competence has been linked to improved health outcomes. Studies have shown that patients who receive culturally competent care experience better health, increased satisfaction with their care, and improved patient-provider relationships. Nurses who are culturally competent are able to:
– Identify and address cultural barriers: They can recognize and mitigate potential cultural barriers that may impact patient care, such as language differences, health beliefs, or social stigmas.
– Provide tailored patient education: They can develop and deliver patient education materials and information that are culturally relevant and accessible to patients.
– Build strong patient-provider relationships: They can establish trust and rapport with patients by demonstrating respect for their cultural values and fostering open communication.
– Collaborate with community partners: They can work with community organizations, cultural healthcare providers, and faith-based groups to bridge healthcare gaps and address social determinants of health.
| Cultural Competence Elements |
Impact on Health Equity |
| Cultural sensitivity |
Promotes patient trust and open communication |
| Cultural knowledge |
Reduces health disparities by addressing culturally specific health needs |
| Cultural skills |
Enhances patient engagement and adherence to care plans |
By fostering cultural competence in nursing, healthcare professionals can contribute significantly to reducing health disparities, improving health outcomes, and promoting health equity for all.
Empowering Nurses as Leaders in the Digital Age
The Changing Landscape of Healthcare
With advancements in technology, the healthcare industry is undergoing a digital transformation. Nurses, as essential healthcare providers, must adapt and embrace these changes to enhance patient care. Wayne State University’s School of Nursing is leading the charge in preparing future nurses for the digital age.
Data-Driven Decision-Making
Empowering nurses with data analytics and artificial intelligence capabilities enables them to make informed decisions. They can access real-time patient information, identify trends, and predict potential outcomes to provide personalized and evidence-based care.
Telehealth and Remote Monitoring
Digital technology has redefined how healthcare is delivered. Nurses can connect with patients remotely through telehealth platforms, increasing access to care, especially in underserved communities.
Advanced Simulation and Virtual Reality
Wayne State SDN 2025 utilizes advanced simulation and virtual reality tools to provide immersive training for nurses. This allows them to develop their clinical skills in a safe and controlled environment.
Interdisciplinary Collaboration
In the digital age, nurses collaborate closely with other healthcare professionals, including physicians, pharmacists, and engineers. This interdisciplinary approach fosters innovative solutions and improves patient outcomes.
Examples of Nursing Leadership in the Digital Age
| Area of Leadership |
Nurses’ Role |
| Telehealth Implementation |
Developing and implementing telehealth programs to enhance access to care
|
| Data Analytics |
Analyzing patient data to identify patterns, predict outcomes, and develop personalized care plans
|
| Virtual Reality Simulation |
Training nurses in advanced clinical skills using immersive virtual reality simulations
|
A Focus on Global Health: preparing nurses for Tomorrow’s challenges
Global Health Nursing Concentrations
The MSN program offers two global health nursing concentrations:
1. Global Health Certificate: Provides a foundation in global health nursing, with a focus on health disparities, cultural sensitivity, and international health policy.
2. Global Health Nurse Practitioner Certificate: Prepares nurses to provide advanced practice nursing care in global health settings, including primary care, maternal and child health, and infectious disease management.
Collaborative Partnerships
The program partners with various organizations to provide students with global health experiences, including:
- World Health Organization (WHO)
- UNICEF
- International Red Cross
These partnerships offer opportunities for students to participate in research, internships, and service-learning projects in global health settings.
Global Health Fieldwork
Students in the global health concentrations are required to complete a field experience in a global health setting. This allows students to apply their knowledge and skills in a real-world context and gain valuable hands-on experience in providing care to underserved populations.
Interdisciplinary Collaboration
The program emphasizes collaboration with other disciplines, such as public health, medicine, and social work, to provide a comprehensive approach to global health issues. Students work with faculty and professionals from diverse backgrounds to develop a deep understanding of the complex factors that influence global health.
Faculty Expertise
The program is led by experienced faculty with expertise in global health nursing, public health, and international development. Faculty engage in cutting-edge research and actively participate in global health initiatives, providing students with access to the latest knowledge and best practices in the field.
Program Structure at a Glance:
| Concentration |
Required Credits |
Fieldwork |
| Global Health Certificate |
12 |
1 credit |
| Global Health Nurse Practitioner Certificate |
21 |
6 credits |
The Future of Nursing Education: Wayne State’s Vision for 2025
Creating a Culture of Innovation
Wayne State’s SDN 2025 vision fosters a culture of innovation and encourages unconventional thinking. The program challenges traditional nursing education practices by embracing technology, interdisciplinary collaborations, and evidence-based approaches.
Transforming the Curriculum
The curriculum has been redesigned to reflect the evolving healthcare landscape and the need for highly adaptable nurses. The program integrates cutting-edge content, experiential learning opportunities, and simulations to prepare students for real-world challenges.
Enhancing Clinical Experiences
Wayne State recognizes the value of hands-on experiences. The program provides students with ample opportunities for clinical immersion in a variety of healthcare settings, ensuring they develop the critical skills and confidence necessary for practice.
Fostering Collaborative Learning
Collaboration is emphasized throughout the program. Students engage in interprofessional projects, peer-to-peer learning, and community-based initiatives to enhance their communication, teamwork, and problem-solving abilities.
Preparing Nurses for Leadership
Wayne State’s SDN 2025 prepares nurses to assume leadership roles in the healthcare system. The program provides opportunities for students to develop their decision-making, advocacy, and mentorship skills, equipping them to make a meaningful impact on patient care and healthcare policy.
Embracing Technology
Technology plays a vital role in nursing education. Wayne State incorporates virtual simulations, online learning platforms, and mobile health technologies into the curriculum to enhance student engagement and prepare them for the rapidly evolving digital healthcare landscape.
Advancing Research and Scholarship
The program emphasizes the importance of research and scholarship to inform evidence-based practice and drive innovation. Students are encouraged to participate in research projects, present their findings at conferences, and contribute to the advancement of nursing knowledge.
A Commitment to Personalized Learning: tailoring programs to meet individual needs
A Focus on Student Success
Wayne State University School of Dentistry (WSU SDN) is dedicated to ensuring the success of each student. Through personalized learning, we tailor our programs to meet individual needs, empowering students to excel in their academic and professional pursuits.
Customized Curriculum
WSU SDN offers a flexible curriculum that allows students to customize their learning paths to align with their goals. Students can select elective courses, research opportunities, and clinical experiences tailored to their interests.
Individualized Advising
Each student is assigned an academic advisor who provides personalized guidance throughout their academic journey. Advisors work closely with students to develop tailored study plans, explore career options, and navigate the complexities of dental education.
Flexible Learning Options
WSU SDN offers a range of flexible learning options to accommodate the diverse needs of our students. These include part-time programs, online courses, and blended learning formats, allowing students to balance their studies with other commitments.
Experiential Learning
We emphasize experiential learning to provide our students with hands-on experience in a variety of clinical settings. Through rotations in our state-of-the-art clinics and partnerships with local hospitals, students develop the skills and confidence they need to succeed as dentists.
Support for Diverse Learners
WSU SDN is committed to supporting diverse learners. We provide accommodations for students with disabilities and offer programs designed to enhance the success of underrepresented groups in dentistry.
Data-Driven Decision Making
WSU SDN uses data-driven decision making to continuously improve our personalized learning initiatives. We track student progress, gather feedback, and make data-informed adjustments to ensure that our programs are meeting the evolving needs of our students.
Student Success Metrics
Our commitment to personalized learning is reflected in our impressive student success metrics:
| Metric |
Value |
| Student retention rate |
95% |
| Graduation rate |
98% |
| Board exam pass rate |
99% |
Building Bridges between theory and practice
Wayne State’s School of Nursing is committed to bridging the gap between theory and practice to prepare students for a successful career in nursing. Through a variety of innovative programs and initiatives, the school is helping students to develop the skills and knowledge they need to provide high-quality patient care.
Clinical Simulation Center
The Clinical Simulation Center provides a state-of-the-art environment for students to practice their skills in a safe and controlled setting. The center is equipped with realistic patient simulators, as well as a variety of other equipment and resources that allow students to experience real-world scenarios.
Interprofessional Education
Wayne State’s School of Nursing is committed to interprofessional education, which prepares students to work effectively with other healthcare professionals to provide comprehensive patient care. Students participate in interprofessional learning activities throughout their program, including team-based projects and simulations.
Community Engagement
The School of Nursing is actively engaged in the community, providing a variety of services to underserved populations. Students have the opportunity to participate in community outreach programs, such as health screenings and educational workshops, to gain hands-on experience and make a positive impact on their community.
Nursing Research
Wayne State’s School of Nursing is a leader in nursing research, with faculty members conducting cutting-edge research in a variety of areas. Students have the opportunity to participate in research projects, which can provide them with valuable experience and help them to develop their critical thinking skills.
Preceptorship Program
The Preceptorship Program is a unique opportunity for students to work one-on-one with an experienced nurse in a clinical setting. Preceptors provide students with guidance and support, as well as the opportunity to observe and practice their skills in a real-world environment.
Simulation-Based Learning
Simulation-based learning is a teaching method that uses realistic simulations to provide students with hands-on experience in a safe and controlled setting. Students participate in simulation exercises throughout their program, which allows them to practice their skills and learn from their mistakes in a non-threatening environment.
Technology-Enhanced Learning
Wayne State’s School of Nursing uses a variety of technology-enhanced learning tools to help students learn and retain information. These tools include online simulations, interactive tutorials, and e-books.
Distance Learning
The School of Nursing offers a variety of distance learning programs that allow students to complete their nursing education from anywhere in the world. These programs are ideal for students who have busy schedules or who live in rural areas.
Continuing Education
The School of Nursing offers a variety of continuing education courses for nurses who want to stay up-to-date on the latest developments in nursing practice. These courses are offered in a variety of formats, including online, in-person, and hybrid.
| Program |
Length |
| Accelerated BSN |
16 months |
| Traditional BSN |
4 years |
| MSN |
2 years |
| DNP |
3 years |
Creating a Collaborative Environment: Fostering Open Dialogue and Teamwork
At Wayne State University, we prioritize the creation of a collaborative and inclusive environment where diverse perspectives are valued and open dialogue is encouraged. To achieve this, we implement various initiatives to foster teamwork and promote effective communication.
Shared Learning Spaces
We provide ample shared learning spaces, such as group study rooms and communal areas, to facilitate student interactions and collaborative projects. These spaces encourage students to engage with each other, share ideas, and build strong working relationships.
Team-Based Projects
Our curriculum incorporates team-based projects that require students to work together to solve problems, exchange knowledge, and develop shared solutions. These projects promote teamwork, enhance communication skills, and foster a sense of collective responsibility.
Peer-Assisted Learning
We offer peer-assisted learning programs where students from different levels of experience work together. Senior students mentor and support junior students, creating a supportive learning environment where all students feel comfortable asking questions and contributing to discussions.
Online Collaboration Tools
We leverage technology to enhance collaboration. Online platforms, such as Canvas and Zoom, provide students with access to virtual meeting spaces, discussion forums, and shared documents. These tools facilitate seamless communication and collaboration outside of the classroom.
Active Listening
We emphasize the importance of active listening and respectful communication in all our interactions. Students are encouraged to listen attentively to each other’s perspectives, ask clarifying questions, and engage in thoughtful discussions.
Diversity and Inclusion
We cultivate a diverse and inclusive environment where students from all backgrounds and identities feel valued and respected. This fosters open dialogue, encourages multiple perspectives, and creates a welcoming learning community for all.
Trust and Respect
Trust and respect are essential ingredients in a collaborative environment. We establish clear expectations for respectful behavior, encourage positive feedback, and provide opportunities for students to build trust and rapport with their peers and instructors.
Conflict Resolution
We equip students with conflict resolution skills to manage disagreements and misunderstandings in a constructive manner. This ensures that conflicts are resolved effectively, preserving positive relationships and maintaining a productive learning environment.
Feedback and Assessment
Regular feedback and assessment not only evaluate student learning but also provide opportunities for ongoing improvement. We encourage students to provide feedback to their peers and instructors, fostering a culture of constructive criticism and mutual learning.
Continuous Improvement
We continually evaluate our collaborative practices and seek opportunities for improvement. By actively listening to student feedback and implementing evidence-based strategies, we aim to create an increasingly inclusive and supportive learning environment.
Wayne State University’s 2025 Strategic Plan: A Vision for the Future
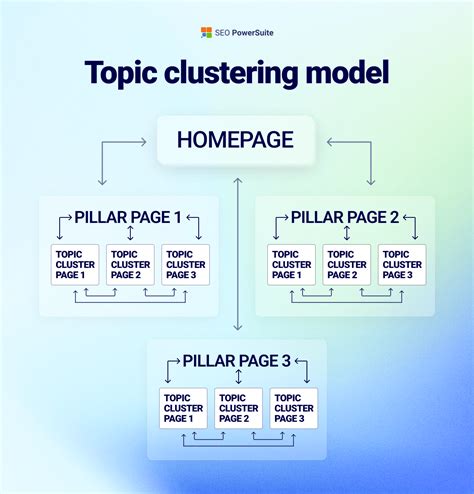
Wayne State University’s 2025 Strategic Plan outlines the university’s vision for the future. The plan is centered around four main pillars: student success, faculty and staff excellence, research and innovation, and community engagement.
The plan sets out a number of ambitious goals for the university, including: increasing the number of students who graduate with a degree, improving the quality of teaching and research, and increasing the university’s impact on the community. The plan also includes a number of initiatives to address the challenges facing higher education, such as the rising cost of tuition and the need to prepare students for the workforce.
The 2025 Strategic Plan is a bold and ambitious vision for Wayne State University. The plan has the potential to transform the university into a leading institution of higher education. However, the plan will only be successful if it is implemented with care and attention. The university must make sure that it has the resources and support to carry out the plan’s goals.
People Also Ask
What is Wayne State University’s 2025 Strategic Plan?
Wayne State University’s 2025 Strategic Plan is a comprehensive plan that outlines the university’s vision for the future. The plan is centered around four main pillars: student success, faculty and staff excellence, research and innovation, and community engagement.
What are the goals of the 2025 Strategic Plan?
The 2025 Strategic Plan sets out a number of ambitious goals for the university, including: increasing the number of students who graduate with a degree, improving the quality of teaching and research, and increasing the university’s impact on the community.
How will the 2025 Strategic Plan be implemented?
The 2025 Strategic Plan will be implemented through a number of initiatives and programs. The university will need to make sure that it has the resources and support to carry out the plan’s goals.